If you ever flipped a cassette with a pencil or blew dust out of a Nintendo cartridge, you know that memory isn’t just what’s stored. It’s also what’s retrieved. For many Gen X and Boomer adults, our most reliable “retrieval cue” has four legs and a tail. A dog that expects the 6 a.m. walk, a cat that appears at the exact sound of a can opener. These rituals mark time, nudge us into motion, and anchor the day. It’s fair to ask: are pets good for memory?
Multiple studies, especially a large, 18-year European study, suggest pet ownership is associated with slower cognitive decline in later life. Dogs are linked to better memory (immediate and delayed recall), and cats to better verbal fluency.
What the strongest evidence shows
A 2025 paper in Scientific Reports followed more than 16,000 adults (50–99) across 18 years in the SHARE study. Researchers found that pet ownership was associated with a slower decline in cognitive scores over time. The most eye-catching detail: species mattered. Dog owners tended to hold on to episodic memory like the ability to learn and recall word lists. Cat owners showed a gentler slope in verbal fluency such as naming as many animals as possible in a minute. Birds and fish didn’t show a reliable benefit. Notably, these associations looked similar across age bands (younger vs. older seniors), suggesting the link isn’t confined to any single slice of later life.
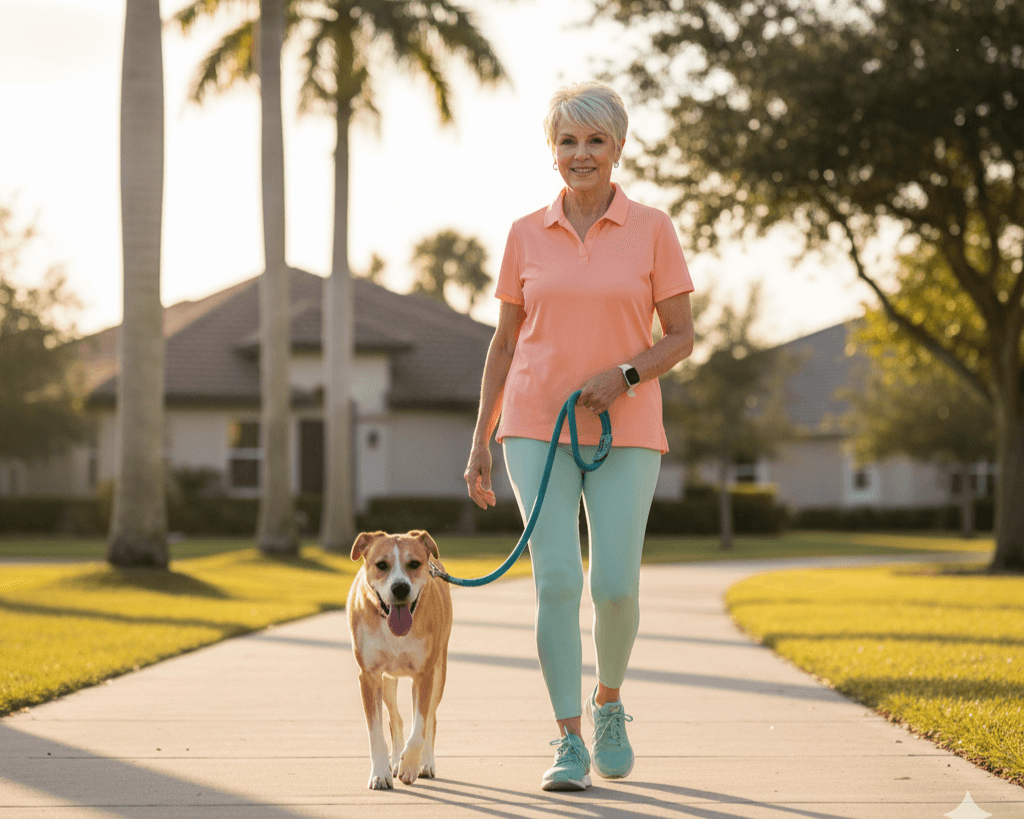
Those patterns echo a common-sense story many of us already experience. Dogs often mean regular walks, schedules, and chats with neighbors; cats provide mentally engaging, socially meaningful companionship at home. Both create routines and predictable cues that help the brain organize, retrieve, and reinforce information.
Memory isn’t isolated, dogs and cats seem to support different cognitive strengths
Memory (especially episodic memory) and verbal fluency are key parts of cognition that age differently. The SHARE analysis suggests dogs may align more with memory maintenance, while cats might align with language-related skills. Why would that be?
- With dogs: Regular physical activity, even a brisk 15-minute loop, supports blood flow, sleep quality, and neuroplasticity, all relevant to memory. Social micro-interactions (“morning,” “great leash!”) add positive mood and mental stimulation.
- With cats: Interactions can be cognitively demanding in a different way such as reading subtle signals, anticipating preferences, and engaging in short, focused play sessions. A lab study using near-infrared spectroscopy showed that cat interactions activate the prefrontal cortex, particularly the inferior frontal gyrus, a region involved in language and social cognition.

Importantly, birds and fish didn’t show the same long-term pattern in SHARE. One proposed reason is that they often involve less reciprocal interaction or may even disturb sleep (e.g., birds), which can undermine memory. The point isn’t that these pets aren’t wonderful, they often bring joy, but that not all pet routines deliver the same cognitive “engagement.”
What about dementia risk?
A large Japanese study took things a step further, looking at incident disabling dementia over about four years. Dog ownership was linked to a lower risk of developing disabling dementia, while cat ownership showed no association. Crucially, the lowest risks were among dog owners who exercised regularly and were not socially isolated, two lifestyle levers we can control, with or without pets. Think of the dog as a compliance partner: you may skip a solo walk, but your dog won’t let you forget.
Brain scans add another layer
Cross-sectional MRI work offers clues about mechanisms. In one study, adult pet owners, especially dog owners, performed better on processing speed, attentional orienting, and story memory, and showed larger volumes in brain networks that support attention, emotion, and internal mentation. Using a model-based “BrainAGE” metric, owners’ brains looked up to ~15 years younger on average. This isn’t proof that pets rewind clocks, but it’s consistent with the idea that the daily structure and engagement pets foster may keep brain networks more robust.
Living alone, living longer—and where pets fit
One repeated finding is that benefits can be strongest for people who live alone. A major UK analysis suggested pet ownership slowed cognitive decline primarily among older adults living alone, a group at higher risk for both loneliness and dementia. If you remember programming the VCR clock solo back in the day, you know that doing life’s logistics alone is different; pets add structure, companionship, and purpose that help counteract the risks of solitary living.

A quick detour on causality (and why it matters)
Correlation isn’t causation; healthier or wealthier people might be more likely to own pets in the first place. The findings are promising but mixed, and we need more research to tease apart what’s causing what. That said, multiple lines of evidence strengthen confidence that pets can contribute to a brain-healthy lifestyle.
Practical takeaways for Gen X & Boomers
Think of pets as habit multipliers—small, consistent nudges that stack up over months and years. If memory is your focus, start with routines that plug straight into what research suggests helps:
- Move with purpose:
- If you have a dog, build a daily walk you can keep (rain plan included: indoor hall laps, mall walking, or backyard fetch circuits).
- No dog? Borrow one, foster short-term or volunteer with a shelter to get the same cue-based activity.
- Make the interaction cognitively rich:
- Dogs: short training refreshers (sit, stay, “find it,” new routes that require navigation).
- Cats: interactive play (wand toys), simple training (targeting, high-five), and puzzle feeders all draw on anticipation and language-adjacent planning that align with verbal fluency networks.
- Guard your sleep:
- If a bird’s dawn chorus or a fish tank’s hum is wrecking sleep, rethink setup. Quality sleep drives memory consolidation.
- Leverage social micro-moments:
- Dog-park greetings and sidewalk chats add up to social stimulation, an already known buffer for decline.
- If you live alone:
- Pets can scaffold routine, purpose, and mood. If full-time ownership is too much, explore “Seniors-for-Seniors” adoption discounts, fostering, or pet-sitting arrangements.
- Know your limits:
- A pet should fit your life, not overload it. The ADDF review emphasizes matching species, and care demands to your capacity. That’s how you can capture benefits without burnout.
What this means for “memory maintenance” in the real world
If you remember carrying quarters for the payphone or the thrill of your first email address, you’re already living proof that memory thrives on meaningful cues and repetition. Pets supply both. Every leash grab, food scoop, or laser-pointer session is a cue that calls up a script. Over time, those scripts reinforce attention, planning, and retrieval, the same mental muscles we use to remember appointments, names, and story details.
The big studies won’t tell you which brand of kibble to buy, but they do suggest the shape of a memory-friendly day:
- Movement anchored by a creature you love
- Brief, engaging challenges (training, play, puzzles)
- Predictable cues at consistent times
- Human contact, even in tiny doses, with people you see because of that pet
Bottom line
The best available evidence links pet ownership with slower cognitive decline, with dogs leaning toward memory benefits and cats toward verbal fluency. A Japanese study connects dog ownership, especially when paired with exercise and social connection, to lower dementia risk. Cross-sectional brain work shows patterns consistent with stronger attention and memory networks among owners. None of this proves pets are memory medicine. But for many Gen Xers and Boomers, pets may be one of the most pleasant, sustainable, and socially meaningful ways to keep the brain’s “record button” active.
If you or someone you love could benefit from reliable help building the daily routines that support memory, safe walks, medication reminders, nutritious meals, and friendly companionship then Happy Mountain Home Care is here to help. Call 954-654-8186 or visit www.happymtn.com to schedule a compassionate, no-pressure conversation about options that fit your life.

Dr. Samantha Montealegre, DNP, PMHNP-BC, is a Board-Certified Psychiatric Mental Health Nurse Practitioner with over 15 years of experience in direct patient care. She brings extensive expertise in family-centered care, ensuring that every client receives compassionate, reliable, and personalized support to enhance their well-being and independence.